I often describe the disease process involved in these cases using the analogy of putting your finger over the end of a garden hose. When you do, the same volume of water comes through as it did without your finger in place, but the aperture is much smaller. This causes changes in the hydrostatic pressure of the flow through the end of the garden hose.
With every heartbeat, there is a sudden surge of fluid through the hole at the base of the skull. This allows the skull to accommodate the increased volume of blood that comes in with every heartbeat. But the change in pressure that happens with the cerebellum herniated (or just crowded) at the base of the skull is just like having your thumb over the end of the garden hose ...
Management of this condition with medications (like prednisone and omeprazole) attempts to reduce the production of spinal fluid. This is analogous to turning down the spigot while keeping your thumb over the end of the garden hose ...
Surgery removes the compression on the cerebellum to allow the fluid to pass through more easily. This is akin to taking your thumb off the garden hose ...
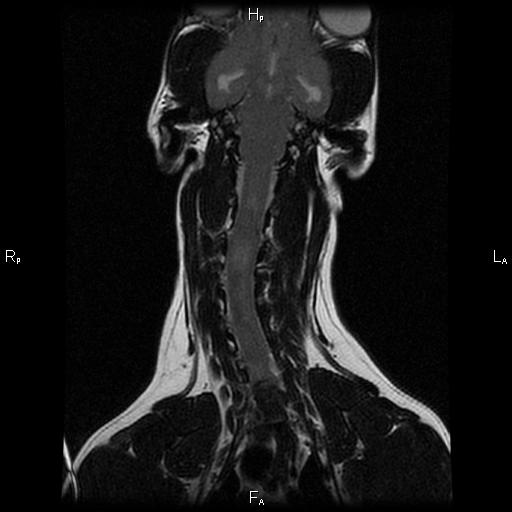
I mention all of this, because I want to remind everyone that surgery doesn't directly make the syringohydromyelia (SM) in the spinal cord go away. Rather, it prevents the disease from getting worse by removing the underlying cause. That's important because it plays into how we define 'success' when looking at surgery.
I always caution my clients to think of a successful surgery as - a patient that recovers from the procedure with no complications and does not get worse over time due to progression of the SM. In other words, these patients may still require medications and the surgery does not (necessarily) make the SM go away. If we get improvement beyond this definition of success, then I call that 'icing on the cake'. Using this definition of success, we are successful with surgery more than 80% of the time.
Most of the surgical failures happen months to years after the procedure due to scar formation at the surgical site. This seems to be where the titanium mesh has its greatest benefit. Since I've been using the mesh, I haven't had any patients worsen in that time frame.
Also, when we remove the bone, there is still a thick membrane (the meninges and particularly the dura mater) that restricts and confines the cerebellum and brain. By patching in a piece of tissue, we can make more room within this membrane and relieve the compression. It's very similar to letting out the waist in a pair of pants. To help prevent scar tissue from forming here and undoing all that we've done, I use tissue collected from the patient's themselves (autograft) rather than material that might cause more inflammation or rejection of the graft.